Fever in the Returned Paediatric Traveller, Part 2
Syndromic Thinking, Smarter Tests, Infection Control Ceasures and Public Health Triggers
Welcome back!
In Part 1, we focused on the power of a GREAT travel history—covering
Geography/ Timing
Risk behaviours and exposures
Eating/ Drinking, Extra precautions
Activities, Accomodation, Age-specific behaviours
Traveller type (VFR, tourism etc) and host factors.
A detailed history, when paired with a careful examination, gives us something invaluable: a clinical syndrome.
Now, in Part 2, we use that clinical syndrome as a springboard into diagnosis, testing, infection control, and public health action.
From Syndrome to Specifics
Clinical syndromes allow us to follow a deliberate and systematic diagnostic approach to identify a specific infectious agent, leading to a more focused evaluation while keeping the differentials open for consideration.

A syndromic approach allows for structured reasoning—narrowing likely pathogens based on:
Incubation periods
Geography
Exposure risks
For example, a fever occurring 2 weeks after returning from travel to India is less likely to be dengue (typical incubation period 4-7 days) and more likely to be malaria, for instance. It is challenging, and perhaps not entirely useful, to provide a comprehensive summary of all infections and their incubation periods; however, knowing the most common infections by region helps keep our focus sharp.
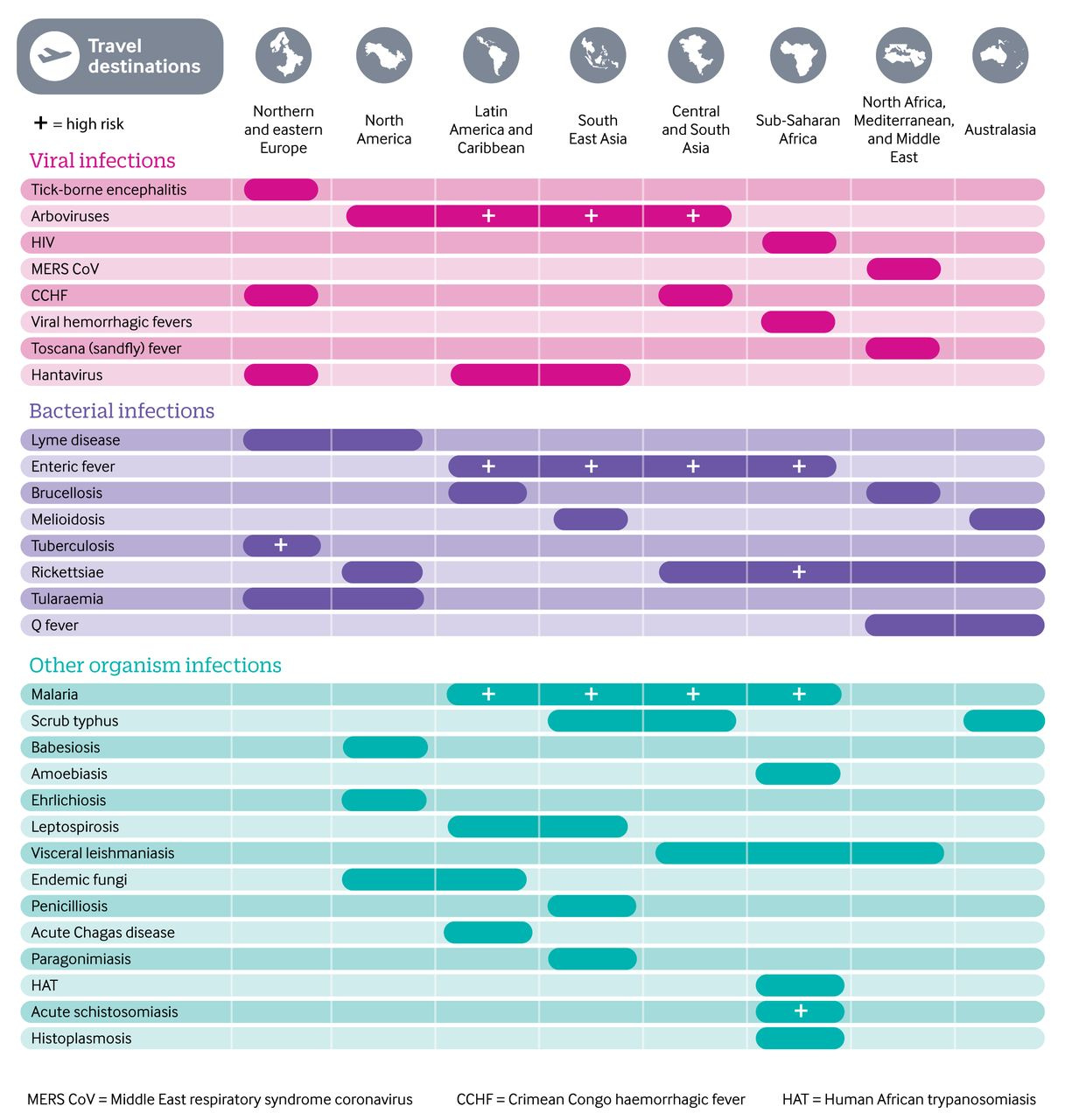
Common Infections by Geographic Region
Adapted from the CDC’s Yellow Book:
Want a visual? Check out the infographic from BMJ: Fink D et al. Fever in the returning traveller. BMJ 2018.
Testing: Start Smart, Then Sharpen Your Focus
Start with first-line investigations applicable to nearly all febrile travellers. These are usually included in most Emergency Department guidelines.
Full Blood Count
Urea, Electrolytes, Creatinine
Liver Function Tests
C-reactive Protein
Blood Cultures
Urine Culture
These help assess severity and hint at certain patterns, though they may be normal in the early phase of illness:
Eosinophilia? Think parasites.
Thrombocytopenia + leukopenia? Think dengue.
Anaemia + high CRP? Think malaria or typhoid.
Next step: Tailor further tests based on syndrome, incubation period and geography. For example:
Fever + CNS symptoms + Respiratory symptoms; 3 days post-return from India. Your options, for example, may include:
Blood
Microscopy- Malaria thin and thick films
Culture- Blood culture
Serology- Dengue serology, Japanese encephalitis virus serology
Molecular- N. meningitidis, S. pyogenes, S. pneumoniae
CSF-
Microscopy- Gram stain, India ink
Culture- CSF culture
Serology- Dengue/ Japanese encephalitis virus serology, etc
Molecular- N. meningitidis, S. pyogenes, S. pneumoniae, HSV; or other multiplex PCR panels e.g. BioFire Meningoencephalitis panel etc.
Respiratory
Microscopy- Induced sputum for acid-fast bacilli (if suspecting TB)
Culture- Sputum culture
Serology- Not useful
Molecular- Respiratory viral PCR
May consider other immunological tests- Tuberculin skin testing or IGRA for TB.
Refer to the Ultimate Guide to Microbiology Test Requests to learn more about selecting the best specimens and test types.
Check out the table for download at the top of the page for common causes of fever in the returned traveller based on clinical syndromes, and the suggested microbiological testing.
Infection Control: Identify and Isolate
The travel history can reveal some clue on risks to the healthcare system, especially if the child has ticked the following checkboxes:
Was hospitalised overseas
Is unvaccinated- think measles!
Was exposed to high-risk settings (farms, refugee camps, sick contacts)
Contact with multi-resistant organisms (MRO)
Recent antimicrobial use
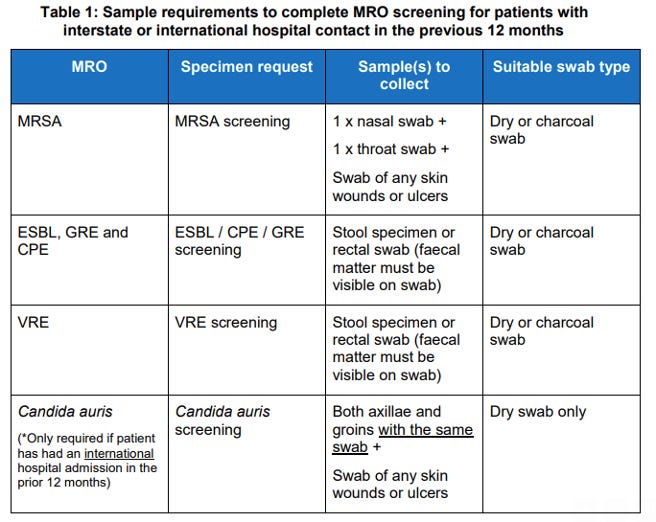
Screening swabs may be indicated in addition to diagnostic tests—check your hospital’s infection control protocol. An example from a hospital where I work:
Public Health: When to Notify
All jurisdictions maintain a list of notifiable conditions:
Urgent notification (e.g. meningococcal disease, measles) → due to high transmissibility and outbreak potential.
Routine surveillance (e.g. pertussis, rotavirus) → notify within 72 hours.
High-consequence threats (e.g. viral haemorrhagic fever) → notify public health and senior leadership immediately upon suspicion.
Be familiar with your local notification form (see example) and reporting timelines.
In the Next Post...
We’ll take a deep dive into travel to Bali, a top destination for WA families. Using the GREAT history, we’ll highlight common infections and high-yield questions to ask.
References:
Fink D, Wani RS, Johnston V. Fever in the returning traveller. BMJ. 2018 Jan 25;360:j5773. doi: 10.1136/bmj.j5773. PMID: 29371218.
Flores MS, Hickey PW, Fields JH, Ottolini MG. A "Syndromic" Approach for Diagnosing and Managing Travel-Related Infectious Diseases in Children. Curr Probl Pediatr Adolesc Health Care. 2015 Aug;45(8):231-43. doi: 10.1016/j.cppeds.2015.06.005. Epub 2015 Aug 5. PMID: 26253891; PMCID: PMC7106018.
Ralph Huits, Davidson H. Hamer, and Michael Libman. Post-Travel Evaluation of the Ill Traveller. CDC Yellow Book: Health Information fro International Travel. Accessed 22nd May 2025. Available online: https://www.cdc.gov/yellow-book/hcp/post-travel-evaluation/post-travel-evaluation-of-the-ill-traveler.html